Prefer listening?
Enjoy an audio version of this article below. Simply press play to listen.
Table of Contents
- What is CBT?
- How Does CBT Work?
- Examples of CBT in Action
- Actionable Steps
- What Will I Be Expected To Do in CBT?
- Resources
- References
What is CBT?
Cognitive Behavioral Therapy (CBT) is widely considered the gold standard approach to therapy.

With over 60 years of research (including randomized control trials), CBT is excellent at treating:
- Depression
- Anxiety
- PTSD
- Substance Use
- Insomnia
- Chronic Pain
- Relationship Difficulties
- Stress
- Eating disorders
How Does CBT Work?
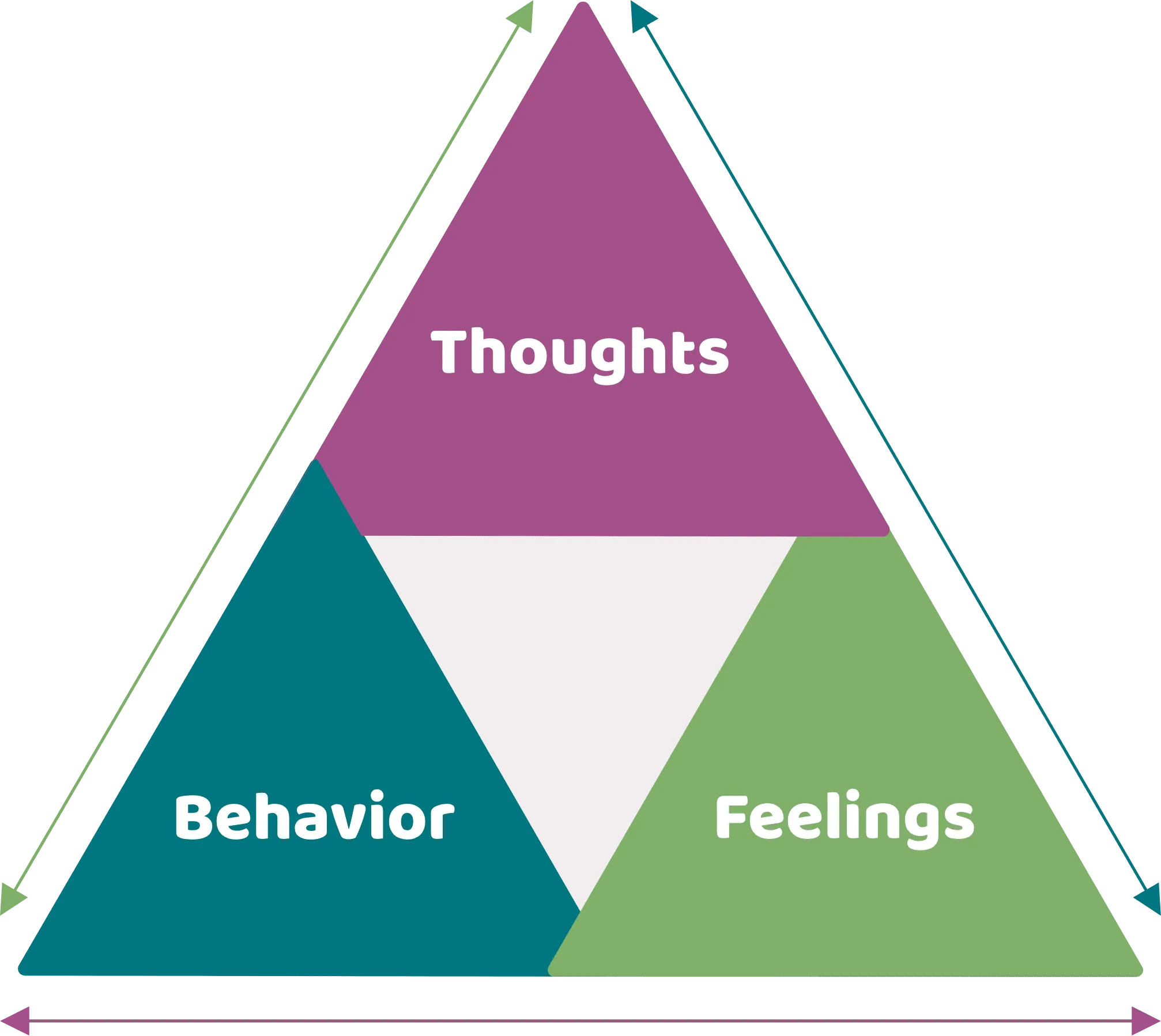
CBT is a collaborative therapy that helps you identify the relationship between what you think, feel, and do. Once you’ve begun to identify those patterns, you can then make shifts to interrupt unhelpful cycles.
The CBT Triangle:
Examples of CBT in Action
Take a look at how Zander, Olivia, and Kevin used CBT to reach their goals and live their most vibrant lives.
Click below to choose a story to read:
Expand All +
Zander is coming into therapy to work on feelings of depression, sadness, and worthlessness. When meeting with their therapist, Zander realized their depression soared after they were asked to redo part of a report. When their boss emailed them on Friday, Zander thought, “I can’t do anything right.” They then began beating themself up until they felt thoroughly defeated. By the time they got home, they decided to cancel their plans. They stayed in bed the rest of the weekend, zoning out on their phone. By the time Sunday came around, Zander began beating themself up all over again because they hadn’t done anything they had planned.
In this example, Zander’s thoughts, emotions, and behaviors become a vicious cycle that gets them caught up in depression.
Zander's CBT Triangle:
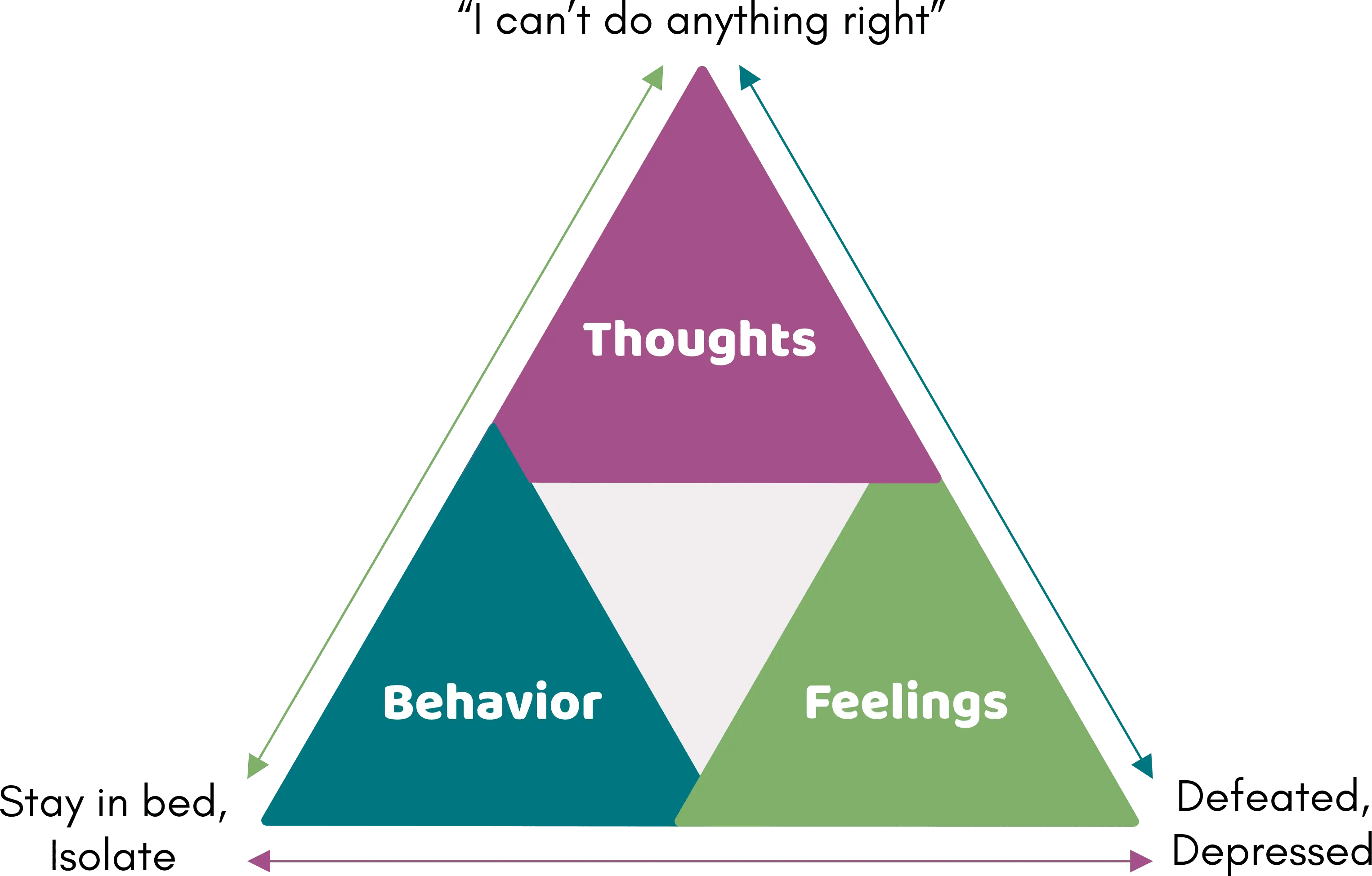
In CBT, Zander learns skills to reevaluate their overly self-critical thoughts, shift behaviors, and identify emotions. Zander learns to question whether the thought “I never do anything right” actually fits the facts. After careful consideration, Zander identifies several areas where they excel as an employee and friend. They also realize they might be exaggerating the importance of being asked to make revisions. In fact, just last week one of their colleagues had been asked to rewrite a report. As they continue therapy, they also work on deeper beliefs around worthlessness and perfection that have fueled their self-criticism over the years.
Zander also works with their therapist to find different ways of dealing with emotions instead of isolating. Zander identifies that avoiding plans last minute usually makes them feel worse. They also identify that staying in bed and scrolling on Instagram for hours also increases their depression. With this information in hand, Zander and their therapist identify other behaviors they could do to get out of their funk. Instead of avoiding the world, Zander learns to create a life they want to live by doing things they used to enjoy. While it was hard in the beginning, they find they actually start enjoying life and are able to nurture important relationships.
By the time Zander leaves therapy, they feel empowered to use the skills they learned in CBT to meet life’s challenges.
Olivia is burned out. While she used to be passionate about her job, she feels like she lost her spark. Olivia used to pride herself at being assigned the hardest tasks. Now she feels overwhelmed as her to-do list grows and calls and emails pour in day and night. At home, Olivia feels even more frazzled as she struggles to keep up with the demands of parenting and the house. She can’t help but think “there must be something wrong with me because I just can’t keep up.” She’s also afraid that she is a “bad mom” for not being able to do all the things the other moms do. She thinks, “I should be able to do it all!” As she pushes herself, she finds herself feeling empty and listless. Things start falling through the cracks as it gets harder to focus.
In this example, Olivia’s thoughts, behaviors, and a difficult work environment are getting her caught up in a spiral of anxiety, depression, and burnout.
Olivia's CBT Triangle:
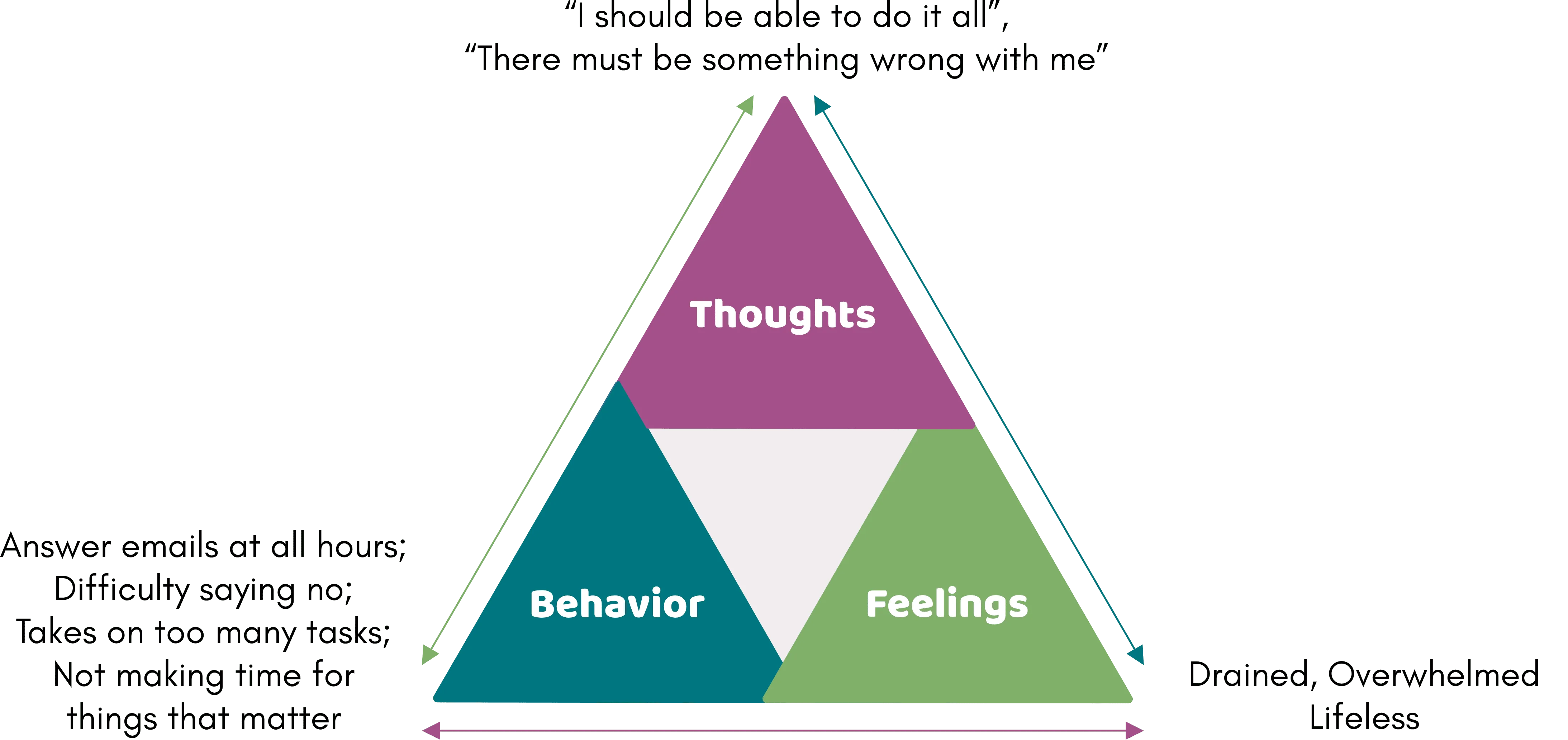
In CBT, Olivia learns to identify the relationship between her thoughts, feelings, and behaviors. Through some exploration, Olivia identifies how telling herself that she should “be able to do it all” and “never say no” is setting herself up for failure. When she believes these things, she puts so much on her plate that she runs herself ragged. While she enjoys the admiration of her colleagues, taking on every project and not prioritizing herself is just feeding her burnout. With the help of her therapist, Olivia identifies that saying “no” to one thing leaves her energy to say “yes” to things that are more important. After role playing with her therapist, Olivia begins saying “no” to additional work responsibilities. She also learns to be okay with doing “good enough” work. She even asks her husband for more help around the house so she could spend more quality time with her kids and relaxing.
As Olivia tracks her emotions and practices saying “no”, she begins to recognize that her work environment is no longer the best fit for her. While she loved the fast paced environment when she was younger and building her career, it isn’t fitting with her priorities now. She doesn’t want to keep grinding herself to the bone. With that information in hand, she begins applying for different jobs that have better work-life balance. While she has to make some compromises, Olivia feels empowered to recognize what she is feeling, say what she wants, and make shifts to her environment so that she can live a life that fits her values.
By learning about the relationship between her thoughts, emotions, and behaviors, Olivia leaves therapy confident in her ability to create her own vibrant life.
Kevin is coming to therapy because he gets anxious in enclosed spaces. After moving into a building with an elevator, Kevin often tells himself “the elevator is going to break down and I’m going to be trapped.” He then becomes so anxious that his face turns bright red and his hands start sweating. On top of his fear of elevators, he now worries other people will notice how he is feeling and judge him for being “so weak.” To avoid it all, Kevin decides he will take the stairs (even though he lives on the 4th floor and carrying up groceries is a pain). Over time, Kevin’s fear of enclosed spaces grows until he is anxious in crowds and even riding in a car with friends.
In this example, Kevin’s thoughts and behaviors (avoidance) keep him from freely living his life.
Kevin's CBT Triangle:
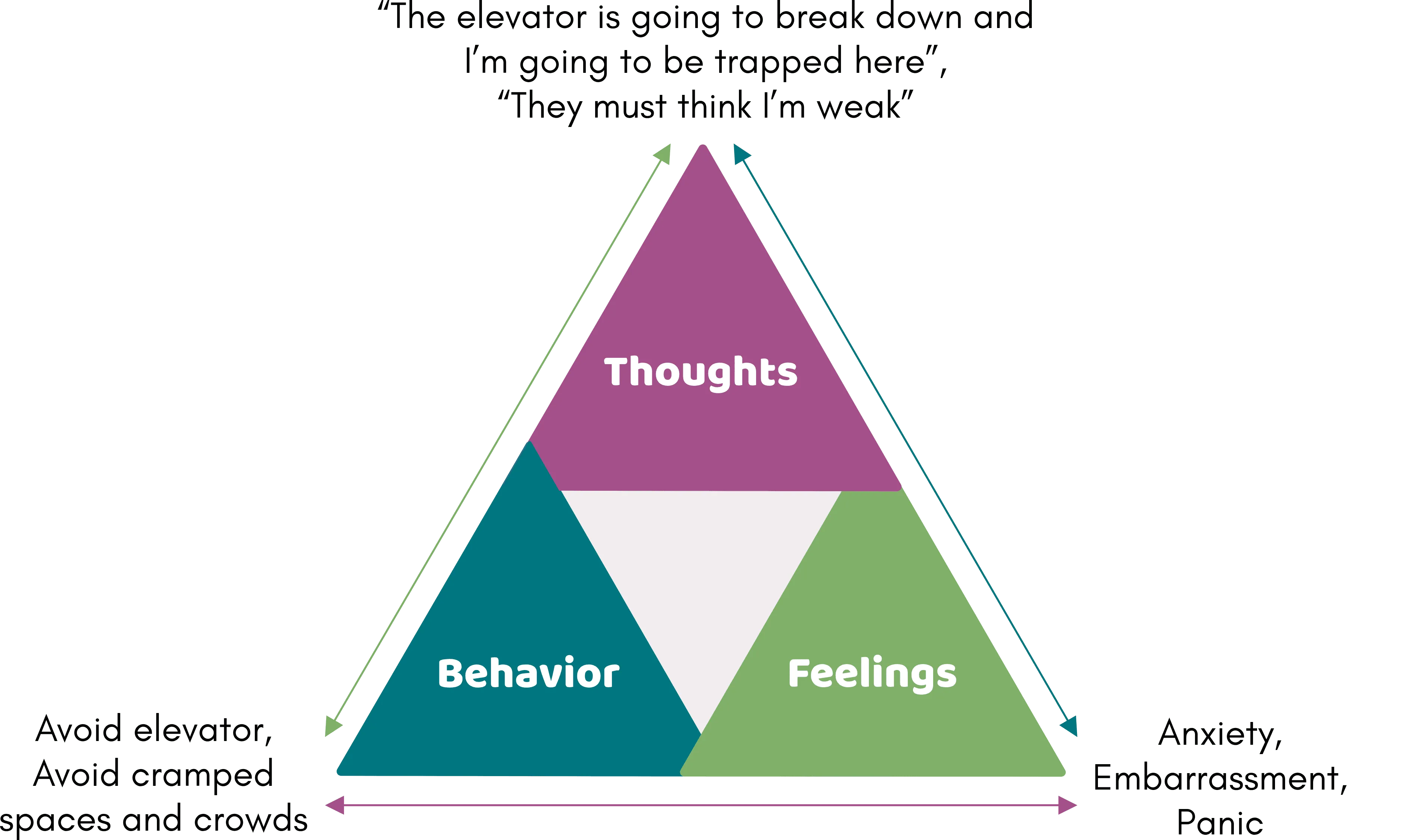
To help Kevin overcome his fears, Kevin and his therapist look at his thoughts around enclosed spaces and being judged. When Kevin takes a step back, he notices that the chances of being caught in the elevator are actually quite low. When he thinks about it, he can only recall a few people who he knows have been stuck in an elevator. He also identifies what he would do if he actually did get stuck in an elevator. While he still feels somewhat anxious, reminding himself of these facts helps lower the anxiety.
Once they work through his thoughts, Kevin and his therapist identify situations where he can challenge his fears. Instead of starting with the elevator (which was the scariest situation on his list), Kevin starts with an easier situation to gain confidence: riding in the car with his brother. Kevin practices this several times until he feels confident. He then practices driving with more people and going into smaller rooms (such as the closet). With practice, Kevin is able to do all of the items on his list. He even begins to feel confident riding in the elevator with multiple people.
By learning to change his thoughts and actions, Kevin is able to challenge his avoidance so he can live life on his terms.
Actionable Steps
In CBT, your therapist will help you learn different skills to help you deal with your thoughts, feelings,and unhelpful behaviors.
Strategies to Shift Thoughts (The Stories We Tell Ourself)
- Track your thoughts, emotions, and behaviors to learn what is keeping you stuck
- Evaluate thoughts based on the evidence (what fits the facts?)
- Learn to identify when you are falling into a problematic pattern of thinking (jumping to conclusions, assuming the catastrophe, etc.)
- Check in on the probability of something bad happening (instead of just assuming)
- Learn to identify whether thought patterns are helpful
- Begin to shift “core beliefs” around worthlessness, helplessness, and unlovability
Strategies to Shift Actions/Behaviors
- Face fears instead of avoiding
- Create a list of fun activities and start doing them
- Learn to say “no” and set boundaries
- Learn to express your needs
- Problem solving (create to do lists, come up with a plan to deal with financial concerns, learn to prioritize tasks, etc.)
- Do “behavioral experiments” to see if your thought is true or if changing what you do changes how you feel
Strategies to Soothe Emotions in the Body
- Identify emotions as they come up and learn how to use them effectively
- Learn the purpose of emotions
- Paced breathing strategies to reduce stress in the body
- Progressive Muscle Relaxation
- Stretching/Yoga
- Mindfulness Techniques
- Find joyful movement (movement that feels good in the body)
What Will I Be Expected To Do in CBT?
Research shows that the individuals who get the most out of therapy are the ones who practice skills in their day-to-day life. For that reason, your therapist will ask you to complete regular practice assignments (like the ones above) to help you reach your treatment goals. With these skills in hand, you will be able to take care of your health and live your most vibrant life.
If you think CBT might be a good fit for you, reach out to Dr. Dautenhahn for a free 15 minute consultation.
Contact Us TodayResources
To learn about Cognitive Behavioral Therapies specifically for PTSD, check out these articles:
To learn about Cognitive Behavioral Therapy for Insomnia, check out this article:
To learn about Cognitive Behavioral Therapy for Substance Use, check out this article:
Other Resources on CBT
- What is CBT? | Making Sense of Cognitive Behavioural Therapy by Mind
- What is Cognitive Behavioral Therapy? by Psych Hub
- Cognitive Behavioral Therapy by the Mayo Clinic
References
Covin, R., Ouimet, A. J., Seeds, P. M., & Dozois, D. J. (2008). A meta-analysis of CBT for pathological worry among clients with GAD. Journal of Anxiety Disorders, 22(1), 108-116.
Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. S. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 58(7), 376-385. doi.org/10.1177/070674371305800702
David, D., Cristea, I., & Hofmann, S. G. (2018). Why cognitive behavioral therapy is the current gold standard of psychotherapy. Frontiers in Psychiatry, 9, 4. doi.org/10.3389/fpsyt.2018.00004
Eng, W., Roth, D.A., & Heimberg, R.G. (2001). Cognitive behavioral therapy for social anxiety disorder. Journal of Cognitive Psychotherapy, 15, 311-319.
Khoo, E. L., Small, R., Cheng, W., Hatchard, T., Glynn, B., Rice, D. B., … & Poulin, P. A. (2019). Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. BMJ Ment Health, 22(1), 26-35.
Svärdman, F., Sjöwall, D., & Lindsäter, E. (2022). Internet-delivered cognitive behavioral interventions to reduce elevated stress: A systematic review and meta-analysis. Internet Interventions, 29, 100553.
Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M., & Cunnington, D. (2015). Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191-204.